Changes in trust in health systems, interactions with the healthcare system, and health-related behaviors and household finances since the COVID-19 pandemic: Preliminary analysis
Principal Investigator

Caroline Rudisill, Associate Professor, Department of Health Promotion, Education, and Behavior, University of South Carolina
Co-Investigators
- Katie Bond, Ph.D. Candidate, Department of Physics and Astronomy, University of Denver
- Anna Chupak, Ph.D. Candidate, Department of Health Promotion, Education, and Behavior, University of South Carolina
- Joan Costa-Font, Professor, Department of Health Policy, London School of Economics
- Sayward Harrison, Associate Professor, Department of Psychology, University of South Carolina
- Peiyin Hung, Assistant Professor, Department of Health Services Policy and Management, University of South Carolina
- Xiaoming Li, Professor, Department of Health Promotion, Education, and Behavior, University of South Carolina
- Luca Salmasi, Associate Professor, Department of Economics and Finance, Università Cattolica del Sacro Cuore
Funded By
Social, Behavioral, and Economic COVID Coordinating Center (SBE CCC)
The Problem
Trust in health systems is integral to the utilization of healthcare and interactions with providers. The COVID-19 pandemic changed individuals’ trust in health systems and caused temporary and permanent changes in healthcare utilization, household finances, and other sectors which ultimately impacted health systems.
This study aims to examine how trust and household finances impacted healthcare utilization and health behavior during the pandemic and the present period, specifically looking at effects across gender, age, and rurality.
The Approach
The research team partnered with Ipsos, an organization that specializes in social and public policy research, to survey 1,085 U.S. residents in July 2020, and 2,189 U.S. residents in May 2023. The survey asked respondents questions about their current beliefs, behaviors, and actions relative to before the pandemic. Survey questions covered five categories: trust in government and health providers, household finances, health literacy, healthcare utilization, and health behaviors.
Ipsos also has demographic information on survey respondents like gender, age, race and ethnicity, working status, household size, and level of education, among others, which were provided to the researchers.
For the analysis, researchers used survey sampling weights to produce nationally representative estimates and perform weighted t-tests across survey years. The team also will use the survey data to produce case-based regression models that predict four healthcare utilization behaviors and three preventative behaviors. The team will examine differences in results across demographics as well.
Next, the team will add health literacy to their analysis (only in the 2023 dataset), using a case-based model to examine different measures of trust (general trust, trust due to social cohesion, trust in different information sources, etc.), demographic effects on trust, and the relationship between trust in health systems and health literacy.
The Findings
The survey found changes in residents’ trust in healthcare systems, government, and household finances from July 2020 to May 2023:
- Trust in healthcare systems: In May 2023, 65.2 percent of respondents reported trusting healthcare systems; about the same as in July 2020 (63.4%).
- Trust in government: There was a significant decrease (29.9% to 19.5%) in respondents that did not trust the national government in July 2020 to May 2023. At the same time, the percent of respondents that did trust the national government increased significantly (32.8% to 44.7%).
- Household finances: There was a significant increase in individuals in May 2023 than in July 2020 reporting much better (5.3% to 8.8%), a little better (11.1% to 15.8%), or much worse (11.4% to 17.6%) finances relative to before the pandemic.
Additionally, the data revealed insights about residents’ healthcare utilization and health behaviors:
- Healthcare utilization: Between July 2020 and May 2023, there was a significant increase (24.9% to 41.3%) in the number of respondents who were more likely than before the pandemic to attend an annual physical. There was also a significant increase (20.5% to 34.8%) in respondents’ likelihood of using pharmacy-based healthcare services. There were no significant changes
in respondents’ likeliness of using virtual or phone-based consultations with their doctors. - Health behaviors: There was an increase in respondents that reported they were much more likely to eat healthy (16.2% to 23.9%) and exercise (16.7% to 22.7%) compared to before the pandemic. However, there were mixed results related to seasonal influenza vaccination, with an increase in respondents saying they were much more likely to get a vaccine (14.0% to 18.9%), and an increase in respondents saying they were somewhat less likely (2.0% to 3.9%) or much less likely (2.7% to 5.7%) to get a vaccine.
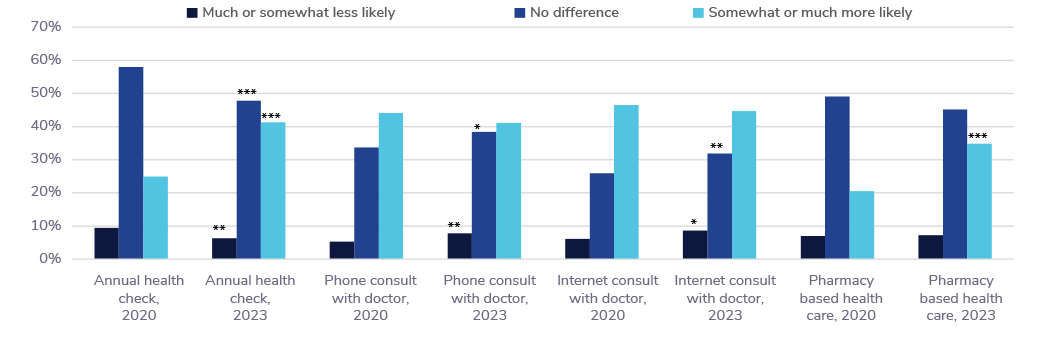
Grouped bar chart showing the number of people who are more likely, less likely, or equally as likely than pre-pandemic to get an annual health check, have a phone consultation with a doctor, have an internet consultation with a doctor, or seek pharmacy based health care, in 2020 and 2023. For discussion, see the findings section.
Selected Publications & Presentations
Chupak, A. L., Rudisill, C., Harrison, S., Linvill, K., Costa-Font, J., Hung, P., & Li, X. (2024). Impact of perceived neighborhood social cohesion on vaccination intentions in the post-pandemic era. Preventive Medicine, 189, 108158. https://doi.org/10.1016/j.ypmed.2024.108158