Stability and volatility in the contextual predictors of working-age mortality before and during the COVID-19 pandemic
Principal Investigator

Shannon M. Monnat
Lerner Chair in Public Health Promotion and Population Health, Director of the Center for Policy Research, and Professor, Department of Sociology, Syracuse University
Co-Investigators
- Jennifer Karas Montez, University Professor, Sociology Department, Syracuse University
- Emily Wiemers, Associate Professor, Public Administration and International Affairs Department, Syracuse University
- Douglas A. Wolf, Professor Emeritus, Public Administration and International Affairs Department, Syracuse University
- Xue Zhang, Lerner Postdoctoral Research Fellow, Syracuse University
Funded By
The problem:
Past research has uncovered wide and longstanding disparities in mortality at the county level in the United States. The contextual predictors of mortality in the U.S. are well-documented, but the COVID-19 pandemic may have upended those associations. In this study, the research team seeks to answer how the importance of county contexts (demographic composition, socioeconomic composition, and population health profiles) and state COVID-19 policies for mortality rates among U.S. adults ages 25-64 fluctuated during the COVID-19 pandemic.
The approach:
Three data sets were used:
1. The National Vital Statistics System restricted-access mortality data from 2018-2021 captured county-level death counts for individuals ages 25-64 by quarter and sex, including all-cause deaths, deaths from drug poisoning, and deaths from COVID-19, adjusted for population;
2. County Health Ranking data from 2018 captured socioeconomic composition, race and ethnic composition, population health profiles (including smoking, obesity, and self-rated health status), and healthcare; and
3. Oxford COVID-19 Government Response Tracker captured states’ COVID-19 policy contexts in 2020 and 2021.
The researchers examined eight county-level factors—education, obesity, self-rated physical health, unemployment, self-rated mental health, median household income, race/ethnicity, and physicians per capita—and two groups of state COVID-19 policies: 1) policies that restricted in-person interactions and 2) policies that provided economic supports.
They analyzed the associations of these factors with three death outcomes:
• all-cause mortality,
• COVID-19 related mortality, and
• drug poisoning mortality.
Using negative binomial regression models, they estimated associations between these county characteristics in 2018, states’ COVID-19 policies, and death rates for each quarter from 2018-2021 for both males and females ages 25-64.
The findings:
For all-cause mortality prior to the pandemic, counties with higher levels of 1) fair/poor self-rated health, 2) mentally unhealthy days, 3) obesity, and 4) Black population shares had higher mortality rates, and counties with higher median household income had lower mortality rates. While these associations were relatively stable from 2018 and 2019, starting in the first quarter of 2020, the observed stability for some factors began to fluctuate. That is, some factors became more strongly associated with mortality during the pandemic than they had been before it, including self-rated physical health, self-rated mental health, and median household income. The importance of county factors fluctuated in correlation with spikes in COVID-19 cases and vaccine uptake.
For COVID-19 related mortality, county self-rated health was a strong predictor until the large-scale rollout of COVID-19 vaccinations in early 2021, after which the associations between county median household income and percentage non-Hispanic Black residents and COVID-19 deaths grew stronger over time. The association between state economic support policies and COVID-19 mortality fluctuated throughout the pandemic; for example, by quarter three of 2021, states with strong economic support policies experienced lower COVID-19 mortality, but by the end of 2021 state economic support policies were no longer associated with COVID-19 mortality.
For drug poisoning mortality, counties with worse mental health prior to the pandemic experienced larger increases in drug overdoses during the pandemic, and mental health became an increasingly important predictor of drug poisoning mortality throughout the pandemic, especially for males.
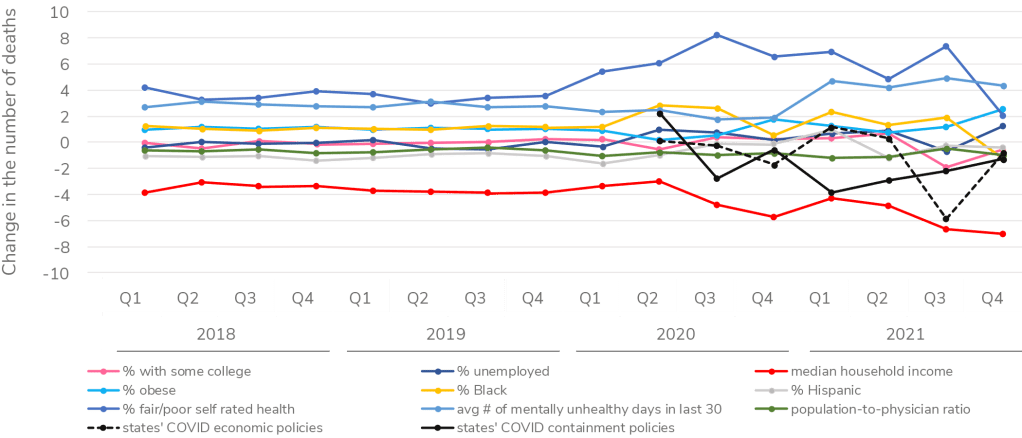
A line graph titled “Estimated change in the number of male (ages 25-64) deaths in an average county for each standard deviation increase in a county context or state policy.” The x-axis displays the years (2018–2021) and quarters (Q1–Q4), and the y-axis reads “Change in the number of deaths” ranging from -10 to 10. Starting in Q3 of 2020, the line graph shows a stronger association between mortality and county self-rated physical health, self-rated mental health, and median household income. It also shows fluctuating associations between mortality and states’ COVID containment policies.
Selected Publications & Presentations
Monnat, S. M. (2021). Rural-Urban Variation in COVID-19 Experiences and Impacts among U.S. Working-Age Adults. The ANNALS of the American Academy of Political and Social Science, 698(1), 111–136. https://doi.org/10.1177/00027162211069717
Monnat, S. M., Wheeler, D. C., Wiemers, E., Sun, Y., Sun, X., Wolf, D. A., & Karas Montez, J. (2023). U.S. States’ COVID-19 physical distancing policies and working-age adult mental health outcomes. Preventive Medicine Reports, 35, 102370. https://doi.org/10.1016/j.pmedr.2023.102370
Montez, J. K., Monnat, S. M., Wiemers, E. E., Wolf, D. A., & Zhang, X. (2024). Stability and Volatility in the Contextual Predictors of Working-Age Mortality in the United States. Journal of Health and Social Behavior, 00221465241271072. https://doi.org/10.1177/00221465241271072
Sun, Y., & Bisesti, E. M. (2023). Political Economy of the COVID-19 Pandemic: How State Policies Shape County-Level Disparities in COVID-19 Deaths. Socius, 9, 23780231221149904. https://doi.org/10.1177/23780231221149902
Wolf, D. A., Monnat, S. M., Wiemers, E. E., Sun, Y., Zhang, X., Grossman, E. R., & Montez, J. K. (2024). State COVID-19 Policies and Drug Overdose Mortality Among Working-Age Adults in the United States, 2020. American Journal of Public Health, e1–e9. https://doi.org/10.2105/AJPH.2024.307621
Zhang, X., & Monnat, S. M. (2024). Watchful, skeptics, and system distrusters: Characteristics associated with different types of COVID-19 vaccine hesitancy among U.S. working-age adults. Vaccine, S0264410X24007217. https://doi.org/10.1016/j.vaccine.2024.06.047