Prediction of all-cause mortality among Medicare beneficiaries aged 65+ years
Principal Investigator

John Hsu
Director of the Program for Clinical Economics and Policy Analysis, Mongan Institute for Health Policy, Massachusetts General Hospital; Associate Professor of Medicine, Department of Medicine, Harvard Medical School; Associate Professor, Department of Health Care Policy, Harvard Medical School
Co-Investigators
- Deborah Blacker, Professor, Department of Epidemiology, Harvard School of Public Health; Professor, Department of Psychiatry, Massachusetts General Hospital
- David Grabowski, Professor, Department of Health Care Policy, Harvard Medical School
- Tamra Keeney, Research Scientist, Mongan Institute, Massachusetts General Hospital and Harvard Medical School
- Joseph Newhouse, Professor, Department of Health Care Policy, Harvard Medical School
- Sharon Lise Normand, Professor, Department of Health Care Policy, Harvard Medical School
- Christine Ritchie, Director of Research, Division of Palliative Care and Geriatric Medicine, Massachusetts General Hospital and Harvard Medical School
- Mary Price, Analyst, Mongan Institute, Massachusetts General Hospital
Funded By
The problem:
The COVID-19 pandemic has stressed health systems, caregivers, and patients, disrupted care delivery, and resulted in millions of deaths. There appeared to be considerable heterogeneity in the adverse effects, with some individuals at higher risk for deaths than others. The pandemic also resulted in a series of emergency policies and delivery changes aimed at mitigating these adverse effects.
In order to understand the actual consequences of the changes, we first must assess the available data and account for varying levels of individual-level risk for adverse events.
The approach:
The researchers used a sample of 132,627 Medicare beneficiaries aged 65 and older from 2016 – 2019 for whom they had detailed, comprehensive information from multiple datasets. They used linked electronic health records and fee-for-service Medicare insurance claims data to collect demographic and clinical variables relevant to mortality, including frailty, serious illness indicators, and insurance subsidies. They added data on deaths from the health system and state death certificates.
The researchers then employed logistic regression models and ensemble machine learning algorithms to predict death in the next 12 months.
Then, using the model built from 2016 – 2019 records, the team predicted all cause mortality during the first year of the pandemic and compared predicted versus actual mortality.
They also examined potential differential mortality with respect to COVID-19 test access (PCR) as well as infection (SARS-CoV-2) during the first year of the pandemic.
The findings:
The number of daily deaths spiked well above the historical trend in April 2020 and reached an initial peak in May 2020. There was a second peak between December 2020 and February 2021 (winter months in Massachusetts). Most of the increase in deaths was concentrated among older residents (data for those aged 64 or less not shown), e.g., 18-23% increase in all-cause mortality (decedents aged 65+ years) during the first year of the pandemic, compared to the prior year. While many deaths occurred in acute care hospitals, there also were large increases in deaths at home, e.g., 31% increase in all-cause mortality among residents aged 65-74 years at the time of death. Among persons living with AD/ADRD, hospital deaths were considerably higher, e.g., 56% increase among residents aged 75-84 years at the time of death; and, deaths at home were higher, e.g., 99% increase among residents aged 65-74 years at the time of death.
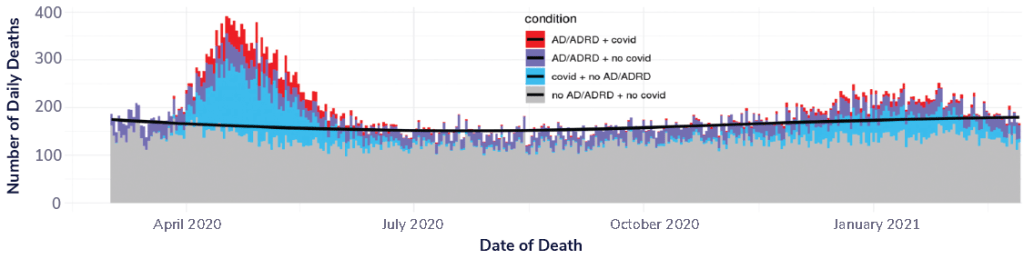
Infographic reading “Daily Deaths in Massachusetts (2020-2021) among residents with or without documented COVID-19, and with or without diagnosed AD/ADRD.”
Selected Publications & Presentations
Hsu, J., Chin, C. Y., Weiss, M., Cohen, M., Sastry, J., Katz-Christy, N., Bertko, J., & Newhouse, J. P. (2021). Growth In ACA-Compliant Marketplace Enrollment And Spending Risk Changes During The COVID-19 Pandemic. Health Affairs, 40(11), 1722–1730. https://doi.org/10.1377/hlthaff.2021.00501
Festa, N., Katz‐Christy, N., Weiss, M., Lisk, R., Normand, S., Grabowski, D. C., Newhouse, J. P., & Hsu, J. (2023). Nursing home infection control strategies during the COVID‐19 pandemic. Journal of the American Geriatrics Society, jgs.18402. https://doi.org/10.1111/jgs.18402
Weiss, M., Normand, S.-L. T., Grabowski, D. C., Blacker, D., Newhouse, J. P., & Hsu, J. (2024). All-cause nursing home mortality rates have remained above pre-pandemic levels after accounting for decline in occupancy. Health Affairs Scholar, 2(11), qxae126. https://doi.org/10.1093/haschl/qxae126