Is there a “new normal” in health system utilization? Describing and analyzing trends following the COVID-19 pandemic
Principal Investigator

Elaine Hill
Professor, Departments of Public Health Sciences and Economics, University of Rochester
Principal Investigator

Meredith Adams
Associate Professor, Anesthesiology, Biomedical Informatics, Pharmacology & Physiology, and Public Health Sciences, Wake Forest University School of Medicine
Co-Investigators
- Daniel Guth, Postdoctoral Fellow, Department of Public Health and Economics, University of Rochester
- Konstantin Kunze, Postdoctoral Fellow, Department of Public Health and Economics, University of Rochester
- Grace Sventek, Predoctoral Research Associate, Department of Public Health and Economics, University of Rochester
Funded By
The problem:
The COVID-19 pandemic had a sizable impact on utilization of healthcare services and mortality. Specifically, there was a significant drop in emergency visits and hospitalizations during COVID-19, but an increase in mortality. Understanding both the causal effect of healthcare utilization on mortality and the potential effect of mortality on healthcare utilization is important to uncover new post-pandemic trends.
This project aimed to:
• quantify the extent to which there exists a “new normal” in healthcare utilization following the COVID-19 pandemic,
• quantify the change in opioid use disorder (OUD)–related healthcare utilization,
• explore mechanisms that may cause this change in healthcare utilization, and
• determine whether there are heterogeneous effects for different populations.
The approach:
Using Medicare and Medicaid claims data from 2018-2022 and National Death Index links for Medicare from 2018-2021 and Medicaid from 2018-2020 to gather cause of death, Hill, Adams, and colleagues analyzed all-cause and opioid-related deaths. They also described national trends in emergency department (ED) visits, inpatient visits, and deaths for each different payer population (Medicare fee-for-service, Medicare Advantage, and Medicaid), separately. In future work, the team will use causal inference methods to quantify the extent to which any reduction in utilization may be due to mortality, enrollment changes, and behavioral changes.
The findings:
An analysis of all services for the Medicare fee-for-service population aged 65 and older revealed an 8 percent decrease in emergency department visits, a 9 percent decrease in hospitalizations, and a 20 percent increase in mortality between the two years before the pandemic (January 2018–February 2020) and the first three years of the pandemic (March 2020–December 2022).
When focusing on OUD-related services in the Medicare fee-for-service population, there was a 24 percent increase in emergency visits, a 27 percent decrease in hospitalizations, and an 11 percent increase in mortality during the same period. However, when limiting the sample to the Medicare fee-for-service population aged 65 and older, the results showed a 20 percent decrease in emergency department visits, a 21 percent decrease in hospitalizations, and no significant decrease in OUD-related mortality. Similar trends were observed for Medicaid enrollees under 65.
The authors suggest that these changes may be attributed to factors such as selection changes—where healthier individuals remained enrolled in insurance during the pandemic—and behavioral changes, like the reduced overuse of emergency department visits due to fear of COVID-19 infection. Analyzing trends in emergency department visits, the researchers focused on two groups: Medicare fee-forservice patients over 65 and Medicaid patients under 65. The study found that while both groups exhibited distinct patterns, all types of ED visits—including emergent non-preventable, emergent preventable, emergent/ primary care treatable, and non-emergent—decreased dramatically. However, these visits showed different trends in their return to normal trajectories.
Using an event study model, the researchers aim to understand the substitutions and tradeoffs in ED visits. Their analyses thus far revealed a statistically significant decrease in ED visits and hospitalizations that began at the onset of the pandemic and persisted through the end of 2022, alongside an increase in mortality rates consistent with the waves of COVID-19 cases.
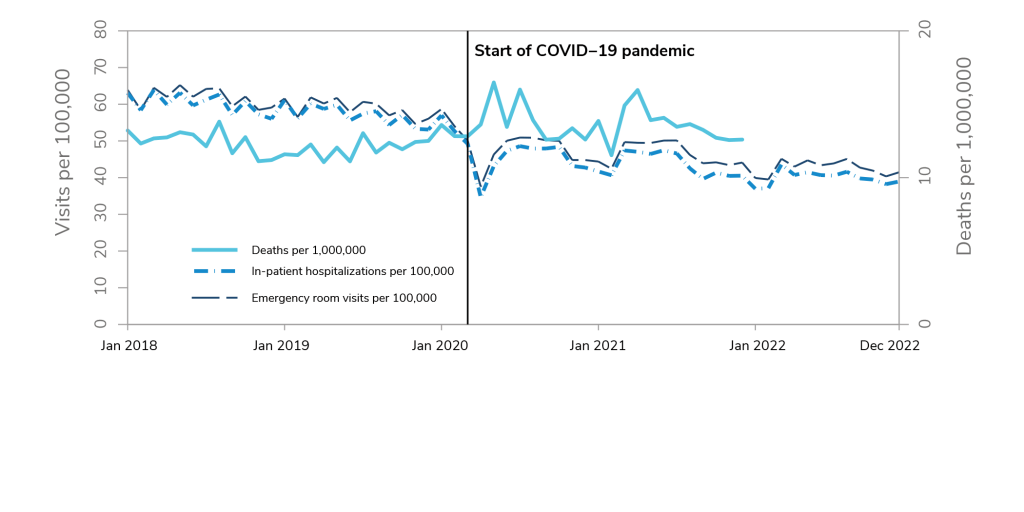
A line graph labeled “Trends in opioid use disorder-related emergency room visits, hospitalizations, and mortality among all Medicare fee-for-service enrollees.” The graph illustrates trends in deaths per 1,000,000 (solid blue line), hospitalizations per 100,000 (dashed blue line), and emergency room visits per 100,000 (dashed black line). The graph has two x axes, one on the left labeled “Visits per 100,000” ranging from 0 to 80 in increments of 10 and one on the right labeled “Deaths per 1,000,000” ranging from 0 to 20 in increments of 10. The y axis represents months from January 2018 through December 2022. OUD-related deaths per 1,000,000 range from about 10 to 15 before March 2020. After March 2020, the line peaks around 16 or 17 in May 2020, June 2020, and April 2021, then returns to baseline by December 2021. OUD-related inpatient and emergency room visits per 100,000 are each between about 55 and 65 before March 2020, reach a low below 40 in April 2020, increase again to about 50, then lower to 40 by December 2022. Overall, the graph illustrates that from the 2 years before the pandemic start to the 3 years after there was a 24% decrease in OUD-related ED visits, a 27% decrease in OUD-related hospitalizations, and an 11% increase in OUD-related mortality.
Selected Publications & Presentations
Hill, E., Mehta, H., Sharma, S., Mane, K., Xie, C., Cathey, E., Loomba, J., Russell, S., Spratt, H., DeWitt, P. E., Ammar, N., Madlock-Brown, C., Brown, D., McMurry, J. A., Chute, C. G., Haendel, M. A., Moffitt, R., Pfaff, E. R., Bennett, T. D., & the RECOVER Consortium. (2022). Risk Factors Associated with Post-Acute Sequelae of SARS-CoV-2 in an EHR Cohort: A National COVID Cohort Collaborative (N3C) Analysis as part of the NIH RECOVER program [Preprint]. Infectious Diseases (except HIV/AIDS). https://doi.org/10.1101/2022.08.15.22278603